Breast cancer surgery is a cornerstone of treatment, offering life-saving potential while balancing the preservation of breast tissue and aesthetics. However, local recurrence after lumpectomy remains a challenge, often linked to residual tumor cells left behind during surgery. Studies reveal that incomplete tumor removal significantly increases the risk of recurrence and necessitates additional procedures, which can burden patients both physically and emotionally.
In response to these challenges, researchers have developed intraoperative fluorescence-guided surgery (FGS) to enhance surgical precision. This technique employs a fluorescent imaging agent, pegulicianine, to illuminate tumor cells during surgery, aiding in real-time detection and removal of residual cancer. In this article, we explore the efficacy, methodology, and implications of fluorescence-guided surgery in breast cancer treatment.
The Need for Precision in Breast Cancer Surgery
While lumpectomy and mastectomy offer similar survival rates, incomplete removal of cancerous tissue during lumpectomy leads to positive margins a strong predictor of local recurrence. Positive margins necessitate reoperation in approximately 20–40% of cases, disrupting treatment plans and increasing patient stress.
Current methods for margin assessment, including post-surgical pathology and frozen section analysis, have limitations:
- Delay in Results: Pathology evaluation may take days, requiring additional surgeries.
- False Positives/Negatives: Tissue deformation and limited sampling can result in inaccuracies.
These gaps underscore the need for advanced intraoperative tools like fluorescence-guided surgery to improve outcomes.
What Is Fluorescence-Guided Surgery (FGS)?
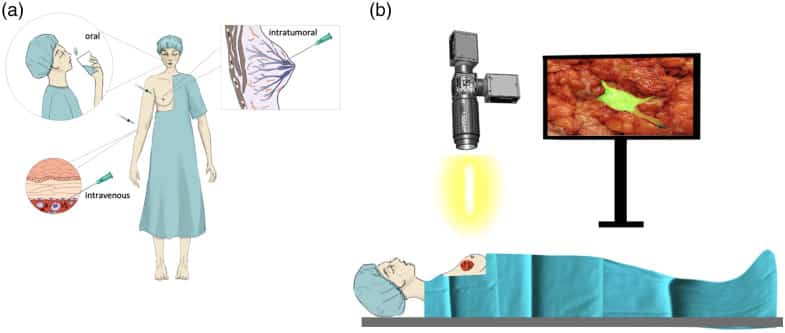
FGS uses a fluorescent agent injected intravenously before surgery. The agent emits a fluorescent signal when activated at tumor sites, allowing surgeons to visualize residual cancer in real time using a handheld imaging probe. This approach minimizes the risk of leaving cancerous tissue behind and reduces reliance on post-surgical pathology.
Key Features of Pegulicianine Fluorescence-Guided Surgery (pFGS):
- Real-Time Imaging: Surgeons can visualize tumor margins intraoperatively.
- Specificity: Pegulicianine is activated only at tumor sites, minimizing false signals.
- Flexibility: Suitable for dense and fatty breasts, as well as invasive and in situ cancers.
Design and Objectives
A prospective, multicenter clinical trial evaluated the safety and efficacy of pFGS in breast cancer surgery. Conducted across 14 U.S. sites, the trial enrolled 406 patients undergoing lumpectomy for stages 0 to 3 breast cancer. Key objectives included:
- Determining the percentage of residual tumor identified by pFGS.
- Assessing sensitivity and specificity of the imaging technique.
- Evaluating its impact on reoperation rates.
Methods
Participants received an intravenous dose of pegulicianine 2–6 hours before surgery. Surgeons performed standard lumpectomies, followed by pFGS imaging. Any fluorescent signal indicating residual tumor prompted additional tissue removal.
- Randomization: Patients were randomly assigned to pFGS or control groups.
- End Points: Coprimary endpoints were residual tumor detection, sensitivity, and specificity.
Results
Tumor Detection and Margin Conversion
- In 7.6% of patients, pFGS identified residual cancer missed during standard lumpectomy.
- For 17% of patients with positive margins, pFGS-guided excision converted 14.5% to negative margins, avoiding additional surgeries.
Sensitivity and Specificity
- Sensitivity: 49.3% across all margins; 58.6% for margins with direct histopathological comparison.
- Specificity: 85.2%, exceeding the prespecified threshold of 60%.
Tissue Volume and Cosmetic Outcomes
The average additional tissue excised using pFGS was 10.1 cm³, an 11% increase over standard lumpectomies. This was lower than the 30% volume increase associated with traditional comprehensive cavity shaving.
Safety
- Adverse Events: Pegulicianine was generally well-tolerated, with a 1.5% rate of adverse reactions.
- Serious Events: Two grade 3 allergic reactions were reported but resolved without lasting effects.
Implications of Fluorescence-Guided Surgery
Improved Surgical Outcomes
FGS enables real-time detection and removal of residual tumors, reducing the need for reoperations and enhancing long-term outcomes. This is particularly beneficial for:
- Patients with dense or fatty breasts.
- Older patients, for whom reoperations pose greater risks.
Enhanced Patient Experience
By minimizing reoperations, FGS reduces:
- Physical and emotional distress.
- Treatment delays and healthcare costs.
Potential for Broader Application
While this study focused on breast cancer, FGS holds promise for other tumor types where residual disease significantly impacts outcomes.
Challenges and Future Directions
Sensitivity Limitations
The trial did not meet the prespecified sensitivity goal of 40% due to design limitations. Future studies with optimized protocols may address this issue.
Adoption and Accessibility
Widespread implementation of FGS will require:
- Cost-effective imaging systems.
- Standardized training for surgeons.
Research Directions
Ongoing trials aim to refine pFGS technology and explore its impact on recurrence rates and cosmetic outcomes.
Conclusion
Intraoperative fluorescence guidance using pegulicianine offers a significant step forward in breast cancer surgery, improving margin assessment and reducing reoperation rates. While challenges remain, this innovative approach has the potential to transform surgical oncology, ensuring better outcomes and a higher quality of life for patients.
By enhancing precision and minimizing residual disease, fluorescence-guided surgery represents a promising advancement in the fight against breast cancer.
FAQs
- What is the primary benefit of fluorescence-guided surgery in breast cancer?
It improves the accuracy of tumor removal during lumpectomy, reducing the risk of reoperations. - Does pFGS work for all types of breast cancer?
Yes, it is effective for both invasive and in situ cancers, as well as dense and fatty breast tissue. - Are there any risks associated with pegulicianine?
Adverse events are rare and typically mild, with allergic reactions being the most common. - How does FGS compare to traditional methods?
FGS offers real-time margin assessment, unlike traditional methods that rely on delayed pathology results. - What are the next steps for FGS research?
Future studies will focus on refining sensitivity, improving technology, and assessing long-term outcomes.
Refrences
Smith BL, Hunt KK, Carr D, et al. Intraoperative fluorescence guidance for breast cancer lumpectomy surgery. NEJM Evid. 2023;2(7). doi:10.1056/EVIDoa2200333
Suurs FV, Qiu SQ, Yim JJ, et al. Fluorescent image-guided surgery in breast cancer using a quenched fluorescence activity-based probe for cysteine cathepsins. EJNMMI Res. 2020;10:111. doi:10.1186/s13550-020-00706-5
Lumicell, Inc. Pegulicianine fluorescence-guided surgery system. ClinicalTrials.gov. 2023. Available at: https://clinicaltrials.gov
Smith BL, Gadd MA, Stone K, et al. Real-time imaging reduces positive margin rates in breast cancer surgery. Ann Surg Oncol. 2023. doi:10.1245/s10434-023-13010-5
van Dam GM, Themelis G, Crane LM, et al. Intraoperative tumor-specific fluorescence imaging in ovarian cancer by folate receptor–α targeting: first in-human results. Nat Med. 2011;17:1315–1319. doi:10.1038/nm.2472


