Triple-negative breast cancer (TNBC) is a complex and aggressive form of breast cancer that accounts for approximately 10–20% of all breast cancer cases. Unlike other breast cancer subtypes, TNBC lacks three key receptors that are commonly used as targets for treatments. This makes TNBC both challenging to treat and unique in its behavior. However, ongoing advancements in research and treatment are offering new hope for those diagnosed with this disease.
In this guide, we’ll explore TNBC in detail from its symptoms and causes to the latest treatment strategies and the steps you can take to improve your outlook.
What Is Triple-Negative Breast Cancer?
TNBC is characterized by the absence of three important receptors on its cells:
- Estrogen Receptors (ER): These receptors fuel cancer growth by binding with estrogen.
- Progesterone Receptors (PR): Similar to ER, these use progesterone to promote growth.
- HER2 (Human Epidermal Growth Factor Receptor 2): A protein that drives rapid cell growth when overproduced.
Since TNBC lacks these receptors, treatments such as hormone therapy (like tamoxifen) and HER2-targeted therapies (like trastuzumab) are ineffective. Instead, systemic therapies like chemotherapy, immunotherapy, and newer targeted therapies are the primary treatment options.
What Makes TNBC Unique?
TNBC tends to grow faster, spread earlier, and has a higher chance of recurrence compared to other breast cancers. Despite this, it is also more likely to respond well to chemotherapy initially.
Key Facts About TNBC:
- Occurrence: Approximately 15% of breast cancer cases.
- Affected Groups: More common in women under 50, Black and Hispanic women, and those with BRCA1 gene mutations.
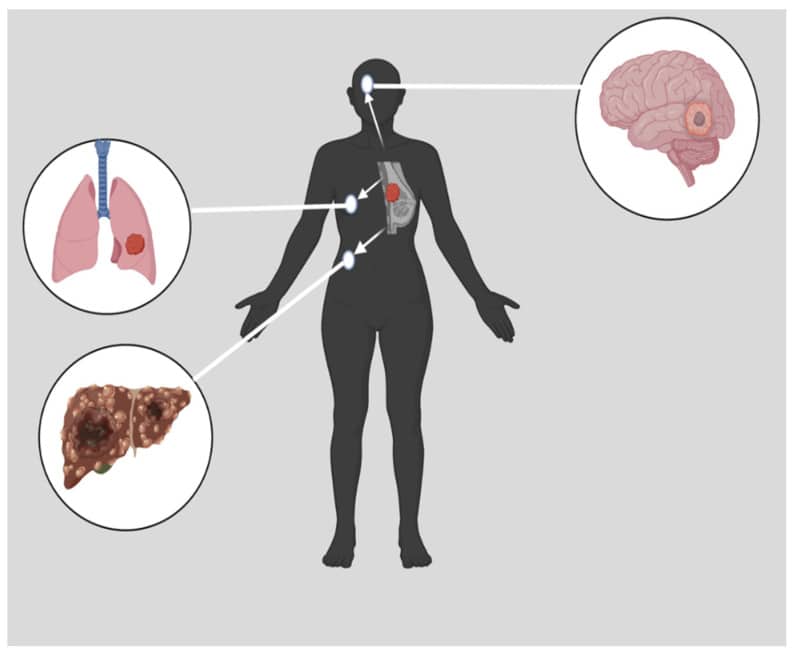
- Aggressiveness: Higher rates of metastasis and recurrence within the first three years after diagnosis.
Who Is at Risk for Triple-Negative Breast Cancer?
Although TNBC can affect anyone, certain factors may increase the likelihood of developing this subtype.
| Risk Factor | Details |
|---|---|
| Age | More common in women under 50. |
| Genetics | Strongly associated with BRCA1 or BRCA2 gene mutations. |
| Ethnicity | Black and Hispanic women are at higher risk compared to white women. |
| Family History | A family history of breast or ovarian cancer increases susceptibility. |
| Lifestyle Factors | Smoking, obesity, and lack of exercise may contribute to risk. |
Symptoms of Triple-Negative Breast Cancer
TNBC shares many symptoms with other types of breast cancer. Common signs include:
- A lump or thickening in the breast or armpit.
- Changes in breast size, shape, or texture.
- Nipple changes, such as inversion or unusual discharge.
- Redness or dimpling of the breast skin (peau d’orange appearance).
- Swelling in lymph nodes under the arm or around the collarbone.
If you notice any of these symptoms, it’s crucial to consult a healthcare provider immediately. Early detection greatly improves treatment outcomes.
Diagnosing TNBC
Accurate diagnosis of TNBC involves a series of tests and evaluations:
- Imaging Tests:
- Mammogram: Detects abnormalities in breast tissue.
- Ultrasound: Helps identify fluid-filled cysts versus solid masses.
- MRI: Provides detailed images of the breast to determine tumor size and location.
- Biopsy:
- A tissue sample is analyzed to confirm TNBC by testing for ER, PR, and HER2 receptors.
- Genetic Testing:
- Identifies mutations in genes like BRCA1 and BRCA2, which influence treatment plans.
- Staging and Additional Tests:
- CT, PET scans, or bone scans may be conducted to check if the cancer has spread.
Stages of TNBC
The stage of TNBC plays a critical role in determining the treatment approach.
| Stage | Description |
|---|---|
| Stage 0 (DCIS): | Noninvasive; cancer cells are confined to ducts and have not spread. |
| Stage I: | Tumor is smaller than 2 cm and hasn’t spread beyond the breast. |
| Stage II: | Tumor is 2–5 cm or has spread to nearby lymph nodes. |
| Stage III: | Locally advanced; tumor has invaded nearby tissues and lymph nodes. |
| Stage IV: | Metastatic; cancer has spread to distant organs like bones, lungs, or liver. |
Treatment Options for Triple-Negative Breast Cancer
TNBC treatment often requires a multi-modal approach due to its aggressive nature. Here’s a closer look at the options:
1. Chemotherapy
- Purpose: Destroys rapidly dividing cancer cells.
- Usage: Often used before (neoadjuvant) or after (adjuvant) surgery.
- Common Drugs: Anthracyclines (doxorubicin), taxanes (paclitaxel), and platinum agents (cisplatin).
2. Surgery
- Lumpectomy: Removes the tumor and a small margin of healthy tissue (breast-conserving).
- Mastectomy: Removes the entire breast, often recommended for larger or multifocal tumors.
3. Radiation Therapy
- Reduces the risk of local recurrence by targeting remaining cancer cells after surgery.
4. Immunotherapy
- Example: Pembrolizumab (Keytruda) boosts the immune system to recognize and attack cancer cells.
- Best For: TNBC tumors that express the PD-L1 protein.
5. Targeted Therapy
- PARP Inhibitors: Olaparib and talazoparib are effective for tumors with BRCA mutations.
- Antibody-Drug Conjugates: Sacituzumab govitecan delivers chemotherapy directly to cancer cells.
What to Expect at Each Stage
| Stage | Treatment Plan |
|---|---|
| Stage I-III (Early): | Surgery combined with chemotherapy, radiation, and sometimes immunotherapy. |
| Stage IV (Metastatic): | Focuses on systemic therapies like immunotherapy, targeted drugs, and palliative care to manage symptoms. |
Living with TNBC
Coping with TNBC requires a holistic approach that addresses physical, emotional, and social needs.
1. Emotional Well-being:
- Join a support group or counseling program for emotional resilience.
2. Self-Care Tips:
- Exercise lightly to combat fatigue.
- Maintain a nutrient-rich diet to support overall health.
3. Stay Informed:
- Explore clinical trials for access to cutting-edge treatments.
FAQs
Q1: Is triple-negative breast cancer curable?
Yes, early-stage TNBC is curable with aggressive treatment.
Q2: What is the survival rate for TNBC?
The 5-year survival rate is:
- 91% for localized TNBC.
- 60% for regional spread.
- 12% for distant metastasis.
Q3: Can I avoid chemotherapy?
Chemotherapy is often essential for TNBC, but alternative treatments may be available in clinical trials.
Q4: Is immunotherapy an option for everyone?
No, it depends on whether the tumor expresses specific proteins like PD-L1.
Conclusion
Triple-negative breast cancer, while aggressive, is increasingly treatable thanks to advances in chemotherapy, immunotherapy, and targeted treatments. Early detection and personalized care play a significant role in improving outcomes. Whether you’re undergoing treatment or managing the emotional and physical challenges, remember that you are not alone.
With the support of medical professionals, loved ones, and resources like clinical trials, there is hope and a path forward. Your strength, paired with cutting-edge science, can help you navigate this journey and emerge stronger on the other side. Stay informed, empowered, and hopeful because brighter days lie ahead.