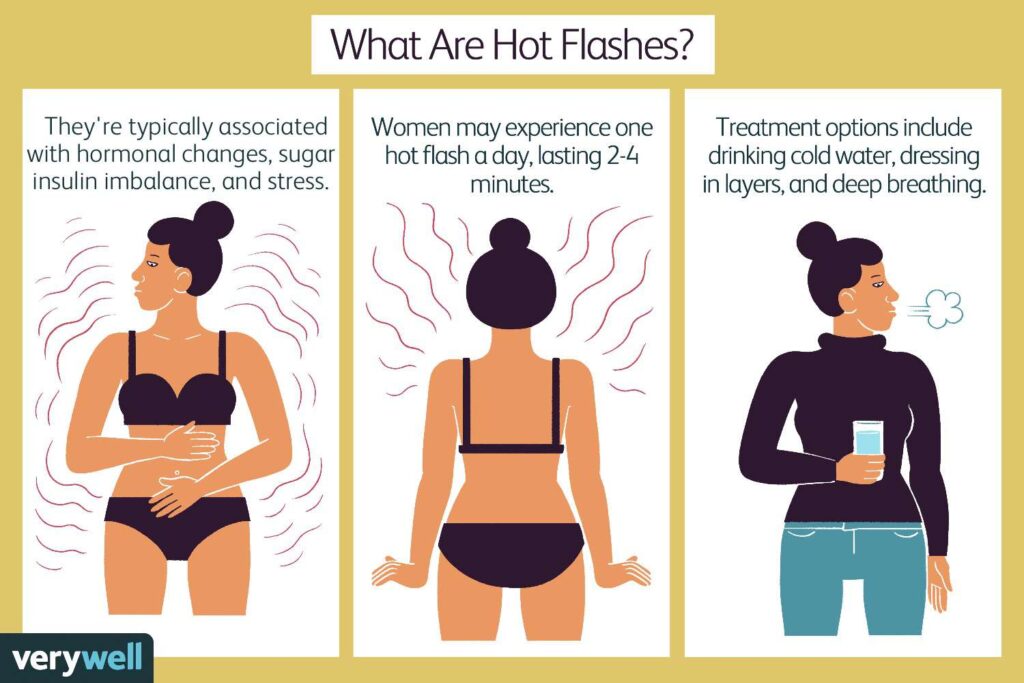
Hot flashes are among the most commonly reported symptoms of menopause, affecting a significant majority of individuals during their transition. However, they aren’t limited to menopause. Factors like hormonal imbalances, medical conditions, certain medications, and even dietary habits can trigger hot flashes. Understanding their causes and treatment options can help you manage them effectively and improve your quality of life.
What Are Hot Flashes?
Hot flashes are sudden episodes of intense warmth, typically concentrated in the upper body, such as the face, neck, and chest. They are often accompanied by:
- Sweating
- Flushing (reddened skin)
- A rapid heartbeat or palpitations
- Tingling sensations in the fingers
- Chills or shivering as the episode subsides
Hot flashes usually last between 30 seconds and 10 minutes but can sometimes extend longer. They may occur sporadically or several times a day, significantly impacting daily routines and sleep when they appear as night sweats.
Causes of Hot Flashes
Hot flashes are associated with hormonal fluctuations, but other triggers and conditions can also lead to similar symptoms:
1. Menopause and Hormonal Imbalances
The most common cause of hot flashes is the hormonal changes associated with menopause.
- Estrogen Decline: A drop in estrogen levels disrupts the hypothalamus (the brain’s temperature regulator), mistakenly signaling that the body is overheating. This triggers sweating and blood vessel dilation to cool the body.
2. Lifestyle and Environmental Triggers
- Spicy Foods and Alcohol: Can stimulate the hypothalamus and mimic hot flash triggers.
- Caffeine: Overconsumption may exacerbate symptoms.
- Smoking: Associated with increased severity and frequency of hot flashes.
- Stress and Anxiety: Elevated cortisol levels from stress can intensify vasomotor symptoms.
3. Medical Conditions
- Hyperthyroidism: Excess thyroid hormone can lead to overheating and sweating.
- Cancer Treatments: Breast and prostate cancer therapies often induce hot flashes by altering hormone levels.
- Neurological Disorders: Conditions like multiple sclerosis and Parkinson’s disease can disrupt the body’s temperature regulation.
4. Medications
Certain drugs, including antidepressants, steroids, and chemotherapy agents, list hot flashes as a side effect.
Who Experiences Hot Flashes?
Hot flashes predominantly affect women undergoing perimenopause and menopause. However, they can also occur in:
- Men: Particularly those undergoing androgen deprivation therapy for prostate cancer or with low testosterone levels.
- Younger Women: Due to premature menopause, thyroid issues, or other hormonal imbalances.
- Transgender Individuals: Hormone therapy or suppression treatments can trigger hot flashes.
Managing Hot Flashes
While hot flashes can be distressing, various lifestyle changes, medical treatments, and natural remedies can help alleviate symptoms.
1. Lifestyle Adjustments
- Dress in Layers: Wear breathable fabrics and easily removable layers.
- Cool the Room: Use fans or air conditioning to keep the environment comfortable.
- Stay Hydrated: Drink plenty of water and avoid overly hot beverages.
- Avoid Triggers: Limit spicy foods, caffeine, and alcohol, which may worsen symptoms.
- Practice Relaxation Techniques: Yoga, deep breathing, and meditation can reduce stress-related hot flashes.
2. Dietary Strategies
Certain foods and nutrients can help reduce hot flash frequency and severity:
- Soy Isoflavones: Found in soybeans, tofu, and miso, mimic estrogen in the body.
- Ginger and Peppermint: Known for soothing the stomach and easing discomfort.
- Cold Foods: Yogurt, salads, and smoothies can provide relief during episodes.
3. Medical Treatments
- Hormone Replacement Therapy (HRT): The most effective treatment for menopausal hot flashes, though not suitable for everyone.
- Non-Hormonal Medications:
- Antidepressants (e.g., paroxetine, venlafaxine)
- Gabapentin (for nighttime symptoms)
- Clonidine (for vasomotor regulation)
- Veozah (fezolinetant): FDA-approved in 2023, this medication targets receptors in the brain to regulate body temperature.
4. Complementary Therapies
- Acupuncture: Some studies suggest it may help reduce hot flash symptoms, though results vary.
- Herbal Supplements: Black cohosh and evening primrose oil are popular, though evidence of their effectiveness is mixed.
When to See a Doctor
If hot flashes interfere with your quality of life or if you experience any of the following symptoms, consult a healthcare provider:
- Hot flashes persist for more than 10 years after menopause.
- Episodes are frequent, severe, or accompanied by symptoms like dizziness or heart palpitations.
- Symptoms of an underlying condition (e.g., thyroid disease, infection).
Hot Flashes and Their Triggers
| Trigger | Description |
|---|---|
| Hormonal Changes | Menopause, pregnancy, or conditions affecting estrogen/testosterone levels. |
| Lifestyle Factors | Smoking, excessive caffeine, spicy foods, alcohol consumption, or stress. |
| Medications | Chemotherapy, antidepressants, steroids, and osteoporosis drugs. |
| Medical Conditions | Hyperthyroidism, neurological disorders, infections, and cancer treatments. |
| Environmental Factors | Hot environments, lack of airflow, and overdressing. |
FAQs
1. How long do hot flashes last?
Hot flashes typically last between 30 seconds and 10 minutes. However, the overall duration of hot flashes (as a symptom of menopause) can range from 7 to 10 years, with some individuals experiencing them longer.
2. Are hot flashes dangerous?
Hot flashes themselves are not harmful, but they can signal low estrogen levels, which are linked to risks such as osteoporosis and cardiovascular disease.
3. Can men experience hot flashes?
Yes, men can experience hot flashes, especially if undergoing hormonal treatments or dealing with conditions affecting testosterone levels.
4. Can hot flashes occur at night?
Yes, hot flashes that occur during sleep are called night sweats and can disrupt sleep quality.
5. Can lifestyle changes help manage hot flashes?
Yes, avoiding triggers, maintaining a healthy weight, staying hydrated, and practicing stress-reduction techniques can help manage symptoms.
Conclusion
Hot flashes are a challenging but manageable symptom for many individuals. Whether caused by menopause, medications, or other factors, a combination of lifestyle adjustments, medical treatments, and natural remedies can offer relief. If hot flashes significantly affect your daily life, consult a healthcare provider to explore tailored treatment options.
By understanding the causes, triggers, and management strategies, you can take proactive steps toward living more comfortably despite these sudden temperature fluctuations.


