Emerging evidence suggests that hormone therapy (HT) may not only alleviate menopause-related symptoms but also slow down biological aging in postmenopausal women. This possibility is backed by new research highlighting the impact of HT on aging markers, mortality risk, and overall health. The findings underline the importance of timing, socioeconomic factors, and personalized treatment plans in optimizing the benefits of HT.
This article delves into the latest studies, exploring how HT influences biological aging, its potential benefits and risks, and what this means for postmenopausal women.
Understanding Biological Aging and Hormone Therapy
Biological aging reflects how well the body functions, as opposed to chronological aging, which is simply the number of years a person has lived. Menopause accelerates biological aging due to a significant decline in estrogen and progesterone levels. These hormonal shifts contribute to symptoms like hot flashes, sleep disturbances, and joint pain while increasing the risk of chronic conditions such as osteoporosis, cardiovascular disease, and cognitive decline.
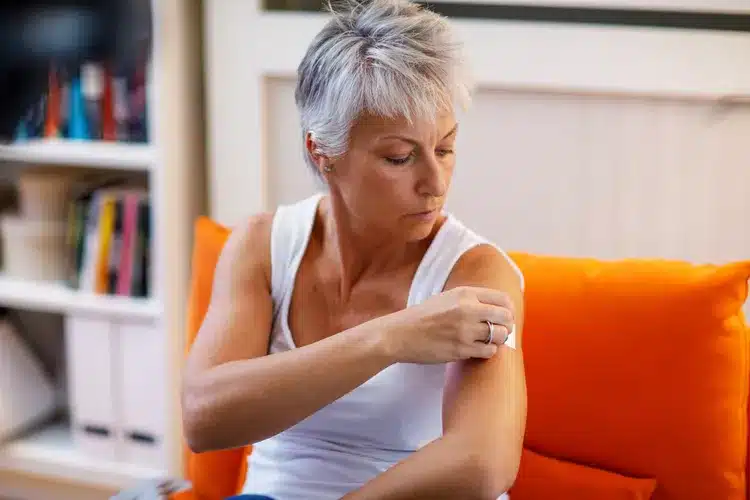
Hormone therapy, also known as hormone replacement therapy (HRT) or menopausal hormone therapy (MHT), replenishes estrogen and progesterone levels to manage menopausal symptoms. Recent studies suggest HT might also play a role in slowing biological aging by reducing inflammation, enhancing metabolism, and supporting overall well-being.
Key Findings on Hormone Therapy and Aging
1. Slowing Biological Aging Through Hormone Therapy
A study analyzing data from over 117,000 postmenopausal women in the UK Biobank found that HT users exhibited slower biological aging compared to non-users. Biological aging was assessed using “phenotypic age,” a marker derived from nine biomarkers associated with mortality risk, including glucose, albumin, and C-reactive protein levels.
Women who had used HT showed an average biological age discrepancy of 0.17 years younger than those who never used it. The benefits were most pronounced in women who started HT after age 50 or used it for 4–8 years, suggesting that timing and duration are critical factors. This biological age reduction corresponds to a 2.25% decrease in all-cause mortality risk and a 5% reduction in cause-specific mortality risk, including cardiovascular and cancer-related deaths.
2. Timing and Duration of Hormone Therapy
The timing of HT initiation plays a pivotal role in its effectiveness. Women who began HT after age 50 experienced the greatest anti-aging benefits, with a biological age discrepancy of 0.32 years younger than non-users. On the other hand, starting HT before age 45 was associated with a 0.33-year increase in biological age, potentially due to the presence of premature menopause or other underlying conditions.
The duration of HT also matters. Women who used HT for 4–8 years showed the most significant reduction in biological aging markers. Prolonged use beyond eight years, however, did not offer additional benefits and may even increase health risks.
3. Addressing Socioeconomic Health Disparities
The research revealed that HT’s benefits were most evident among women from lower socioeconomic status (SES) backgrounds. These women typically experience faster biological aging due to factors like financial stress, limited access to healthcare, and chronic stressors associated with lower income and education levels. HT helped narrow the aging gap between lower-SES women and their higher-SES counterparts, highlighting its potential to reduce health disparities.
Chronic stress accelerates aging by increasing inflammation and oxidative stress. By stabilizing hormonal levels, HT can counteract some of these effects, making it especially beneficial for women facing higher levels of socioeconomic stress.
4. Broader Health Benefits of Hormone Therapy
In addition to slowing biological aging, HT offers other health benefits:
- Bone Health: Estrogen loss after menopause accelerates bone density decline, increasing the risk of osteoporosis and fractures. HT helps maintain bone density and reduces fracture risk.
- Cardiovascular Health: Estrogen has protective effects on the heart and blood vessels, potentially lowering the risk of cardiovascular disease when HT is initiated early.
- Cognitive Function: Improved sleep and mood associated with HT may enhance mental clarity and cognitive performance.
- Skin and Hair: While not a primary indication, some women report improved skin elasticity and hair thickness during HT.
The Risks and Controversies Surrounding Hormone Therapy
Despite its benefits, HT is not without risks. Concerns stem from earlier studies, particularly the Women’s Health Initiative (WHI) in the 1990s, which suggested that HT increased the risk of breast cancer, blood clots, stroke, and dementia. Subsequent re-analyses found that these risks depend heavily on the timing of HT initiation, with younger women (within 10 years of menopause onset) experiencing fewer adverse effects compared to older women.
Potential Risks of Hormone Therapy
- Breast Cancer: Long-term use of combined estrogen-progestin therapy is linked to a higher risk of breast cancer.
- Cardiovascular Events: Older women initiating HT beyond 10 years after menopause face a higher risk of stroke and heart attack.
- Dementia: Late initiation of HT has been associated with an increased risk of cognitive decline.
Balancing Benefits and Risks
The decision to use HT should be individualized, considering the woman’s age, health status, and specific symptoms. For younger women experiencing severe menopausal symptoms, the benefits of HT often outweigh the risks, especially when used for a limited duration.
Who Should Consider Hormone Therapy?
Ideal Candidates
- Women in perimenopause or early postmenopause (within 10 years of menopause onset).
- Those experiencing severe symptoms such as hot flashes, night sweats, or vaginal dryness.
- Women at high risk for osteoporosis or who have already experienced significant bone loss.
Who Should Avoid HT?
- Women with a history of breast cancer, blood clots, or stroke.
- Those with advanced age or who are more than 10 years past menopause onset.
Non-Hormonal Alternatives
For women unable to use HT, lifestyle changes and alternative therapies can provide relief:
- Diet and Nutrition: Consuming a balanced diet rich in calcium, vitamin D, and phytoestrogens (found in soy and flaxseed) can support bone and cardiovascular health.
- Exercise: Regular physical activity, including strength training and weight-bearing exercises, helps maintain bone density and cardiovascular fitness.
- Stress Management: Practices like yoga, meditation, and mindfulness can alleviate mood swings and improve sleep.
- Non-Hormonal Medications: Selective serotonin reuptake inhibitors (SSRIs) and gabapentin are sometimes prescribed to manage hot flashes and mood changes.
The Role of Healthcare Providers
Healthcare providers play a critical role in guiding women through the decision-making process for HT. Key considerations include:
- Thorough Assessments: Evaluating medical history, family history, and current health risks before prescribing HT.
- Personalized Plans: Tailoring HT to individual needs, considering the timing of initiation, duration of use, and choice of hormone formulation (e.g., patches, pills, or creams).
- Regular Monitoring: Conducting routine health checks, including mammograms and bone density scans, to monitor for potential side effects.
Future Directions in Hormone Therapy Research
The findings from the UK Biobank study open avenues for further exploration into HT and its impact on biological aging:
- Long-Term Studies: More randomized controlled trials are needed to establish causation and evaluate long-term safety.
- Precision Medicine: Advances in genetics and biomarkers could enable more personalized HT regimens, maximizing benefits while minimizing risks.
- Addressing Disparities: Research should focus on how HT can be made accessible to disadvantaged populations, addressing systemic barriers to care.
Conclusion
Hormone therapy offers significant promise in managing menopausal symptoms and promoting healthy aging. By slowing biological aging, it may reduce mortality risks and improve quality of life for postmenopausal women. However, its use requires careful consideration of timing, duration, and individual health factors.
As the global population ages, understanding and optimizing treatments like HT will be crucial in addressing the unique challenges faced by postmenopausal women. For now, women are encouraged to consult healthcare providers to determine whether HT aligns with their health goals and needs, ensuring informed, individualized care.
This era of personalized medicine holds hope for empowering women to navigate menopause with confidence and vitality while embracing the opportunities of healthy aging.
FAQs
1. What is hormone therapy (HT)?
HT involves using estrogen, with or without progesterone, to alleviate menopausal symptoms like hot flashes and vaginal dryness.
2. Can HT slow biological aging?
Research suggests HT may slow biological aging by reducing inflammation and supporting overall well-being, especially when started at the right time.
3. What are the risks of HT?
HT carries risks, including breast cancer, stroke, and blood clots, especially when used for long durations or started late.
4. Who should avoid HT?
Women with a history of breast cancer, stroke, or blood clots should generally avoid HT. Consult a healthcare provider to assess personal risks.
5. Are there alternatives to HT?
Yes, options include lifestyle changes, non-hormonal medications, and natural remedies like acupuncture or herbal supplements.
References
- Liu Y., Li C. “Hormone Therapy and Aging,” JAMA Network Open, 2024.
- North American Menopause Society. “HT Position Statement,” 2024.
- Women’s Health Initiative. “HT Risks and Benefits,” NIH, 2022.
- UK Biobank Study. “HT and Biological Aging,” 2024.
- Ruiz GT, Vaughan D. “HT and Health,” Clinical Endocrinology, 2024.