Menopause is a natural biological transition that occurs in every woman’s life. While it signifies the end of reproductive years, it also marks the beginning of significant changes in hormone levels, particularly estrogen. These changes have far-reaching impacts on a woman’s health, notably increasing the risk of cardiovascular disease (CVD). Understanding the connection between menopause, cardiovascular health, and preventative strategies is essential to help women navigate this life stage more effectively.
The Protective Role of Estrogen in Heart Health
Estrogen plays a critical role in maintaining cardiovascular health. Its protective effects extend across several key areas, such as:
- Cholesterol Regulation
Estrogen helps regulate cholesterol levels by:- Increasing high-density lipoprotein (HDL) cholesterol, often called “good cholesterol,” which helps remove bad cholesterol from the bloodstream.
- Reducing low-density lipoprotein (LDL) cholesterol, which contributes to the buildup of fatty deposits in arteries.
- Artery Health
Estrogen keeps blood vessels flexible, allowing them to expand and contract easily, which aids in maintaining healthy blood pressure and preventing arterial damage. - Blood Sugar Control
Estrogen supports glucose metabolism, helping the body effectively regulate blood sugar levels and reducing the risk of insulin resistance.
During menopause, as estrogen levels decline, women lose these protective benefits, leading to:
- Increased cholesterol levels.
- Stiffer blood vessels, raising blood pressure.
- A heightened risk of fat accumulation in arteries, contributing to atherosclerosis (artery narrowing).
These changes collectively increase the risk of coronary heart disease (CHD), heart attacks, and strokes.
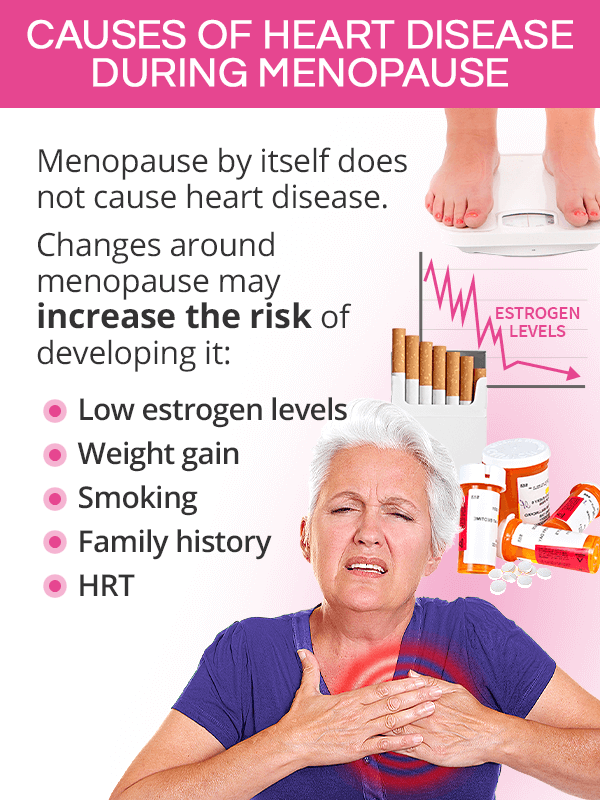
How Menopause Increases Cardiovascular Risks
1. Weight Gain and Abdominal Fat
Weight gain during menopause, particularly around the abdomen, is a common challenge. Visceral fat, which accumulates around the organs, is metabolically active and contributes to chronic inflammation, insulin resistance, and an elevated risk of heart disease.
2. Cholesterol Imbalances
The decline in estrogen often leads to increased LDL cholesterol and decreased HDL cholesterol levels, significantly raising the risk of atherosclerosis and subsequent heart conditions.
3. Impaired Glucose Regulation
Reduced estrogen levels impact the body’s ability to regulate blood sugar, making women more susceptible to insulin resistance and Type 2 diabetes, both of which are major contributors to heart disease.
4. Increased Blood Pressure
As estrogen levels drop, blood vessels lose elasticity, making them stiffer and less responsive to blood flow changes. This increases blood pressure and contributes to hypertension, a key risk factor for cardiovascular disease.
5. Fat Around the Heart
Studies show that postmenopausal women tend to accumulate more fat around the heart, which is strongly linked to coronary artery disease.
Early Menopause and Cardiovascular Risks
Women who experience menopause before the age of 45 (early menopause) face an even greater risk of cardiovascular disease. Prolonged exposure to low estrogen levels increases the likelihood of developing CHD and other cardiovascular conditions.
What Can Women with Early Menopause Do?
- Monitor health closely: Regular checkups to assess cholesterol, blood pressure, and glucose levels are essential.
- Discuss HRT options: Hormone replacement therapy (HRT) may help mitigate the risks associated with early menopause by replacing the estrogen lost prematurely.
Symptoms of Menopause Mimicking Heart Problems
Many symptoms of menopause, such as hot flashes, palpitations, and fatigue, can be mistaken for signs of heart conditions. This overlap can lead to confusion or unnecessary worry.
Common Menopausal Symptoms That Resemble Heart Issues:
- Heart Palpitations: A racing or irregular heartbeat is a frequent menopausal symptom, often caused by fluctuating hormone levels.
- Chest Discomfort: While menopause-related, it’s important to rule out potential heart issues if chest pain occurs.
- Brain Fog and Fatigue: These can be mistaken for signs of poor circulation or heart problems but are often linked to hormonal changes.
Action Step: If these symptoms persist or worsen, consult a healthcare provider to distinguish between menopause-related changes and underlying cardiovascular conditions.
Recognizing a Heart Attack in Women
Heart attacks in women can present differently than in men, often with subtler or atypical symptoms. Knowing these signs is crucial for early intervention:
- Chest pain or discomfort, which may feel like pressure or heaviness.
- Pain radiating to the arms, neck, jaw, back, or stomach.
- Shortness of breath, lightheadedness, or nausea.
Key Tip: If you or someone you know experiences these symptoms, call emergency services immediately.
The Connection Between Hormone Replacement Therapy (HRT) and Heart Health
HRT replaces the hormones that naturally decline during menopause, primarily estrogen. Its impact on cardiovascular health has been a topic of significant research and debate.
Potential Benefits of HRT:
- Cholesterol Regulation: HRT may improve lipid profiles by reducing LDL cholesterol and increasing HDL cholesterol.
- Arterial Health: It can help maintain vascular elasticity, reducing hypertension risks.
- Bone Health: Estrogen helps maintain bone density, lowering the risk of fractures that can indirectly affect cardiovascular health.
Risks Associated with HRT:
- Blood Clots and Strokes: Oral HRT slightly increases the risk of venous thromboembolism (blood clots) and stroke.
- Breast Cancer: Long-term HRT use, especially combined estrogen-progesterone therapy, is linked to a higher risk of breast cancer.
Who Should Consider HRT?
HRT is most beneficial for women:
- Within 10 years of menopause or under age 60.
- With minimal cardiovascular risk factors.
- Experiencing severe menopausal symptoms that affect quality of life.
For women with a history of breast cancer, stroke, or heart disease, alternative treatments should be explored.
Preventative Strategies for Cardiovascular Health During Menopause
The menopausal transition offers a critical window for implementing heart-healthy lifestyle changes.
1. Healthy Eating
Adopting a balanced diet can significantly reduce CVD risk:
- Limit saturated and trans fats: Replace butter with olive oil and choose lean protein sources.
- Increase fruits, vegetables, and whole grains: These provide fiber, antioxidants, and nutrients that support heart health.
- Reduce salt intake: Helps manage blood pressure.
- Incorporate calcium and vitamin D: Essential for maintaining bone and vascular health.
2. Regular Physical Activity
Exercise is a cornerstone of heart health. It helps:
- Maintain a healthy weight.
- Lower blood pressure and cholesterol.
- Improve insulin sensitivity.
Recommendations:
- Aim for 150 minutes of moderate aerobic activity (e.g., walking, cycling) weekly.
- Include strength training to preserve muscle mass and bone density.
3. Weight Management
Excess weight, especially abdominal fat, is a significant risk factor for CVD.
- Monitor portion sizes and avoid high-calorie, low-nutrient foods.
- Gradually incorporate healthier food choices and physical activity into your routine.
4. Smoking Cessation
Smoking doubles the risk of heart attack and accelerates arterial damage. Women going through menopause often find quitting challenging, but support groups and nicotine replacement therapies can help.
5. Alcohol Moderation
Excessive alcohol consumption increases blood pressure and cholesterol. Limit intake to fewer than 14 units per week and consider alcohol-free alternatives.
6. Stress Management
Chronic stress contributes to hypertension and heart disease. Techniques like yoga, meditation, and cognitive behavioral therapy can help reduce stress and menopausal symptoms such as hot flashes and mood swings.
Importance of Routine Screenings
Health Checks During and After Menopause:
- Blood Pressure: Monitor for hypertension.
- Cholesterol Levels: Keep an eye on LDL, HDL, and triglycerides.
- Glucose Levels: Screen for insulin resistance or diabetes.
- Coronary Artery Calcium (CAC) Scans: These can detect early signs of plaque buildup in the arteries, offering insights into heart attack risks.
Why Early Intervention Matters
The menopausal transition represents a unique opportunity for early CVD prevention. Studies suggest that the earlier women adopt heart-healthy habits, the greater their long-term cardiovascular benefits.
Key Preventative Measures:
- Start Small: Introduce manageable changes, such as a daily walk or replacing one unhealthy snack with a healthier option.
- Seek Support: Work with a healthcare provider to create a personalized plan.
- Educate Yourself: Understand your specific risk factors and how to mitigate them.
Conclusion
Menopause is a natural phase of life, but it brings with it an increased risk of cardiovascular disease due to hormonal changes. By adopting heart-healthy lifestyle habits and staying informed about medical options like HRT, women can effectively manage these risks.
Key Takeaway: Menopause is not just an end but an opportunity a chance to prioritize long-term heart health and improve overall well-being.
Resources for Further Support
- The Menopause Charity: menopausecharity.org
- American Heart Association: heart.org
- The Balance App: Personalized menopause symptom management.
- Daisy Network: Support for women experiencing early menopause: daisynetwork.org
- NHS Menopause Support: nhs.uk/menopause


