If you’ve ever found yourself (or someone else) wandering around the house, moving furniture, or even attempting to cook while asleep, you’ve encountered sleepwalking formally known as somnambulism. It might sound like something out of a movie, but sleepwalking is a real phenomenon that affects many people, often leaving them and their loved ones confused or concerned. Let’s explore what causes sleepwalking, how it connects to mental health, and what you can do about it.
What Is Sleepwalking?
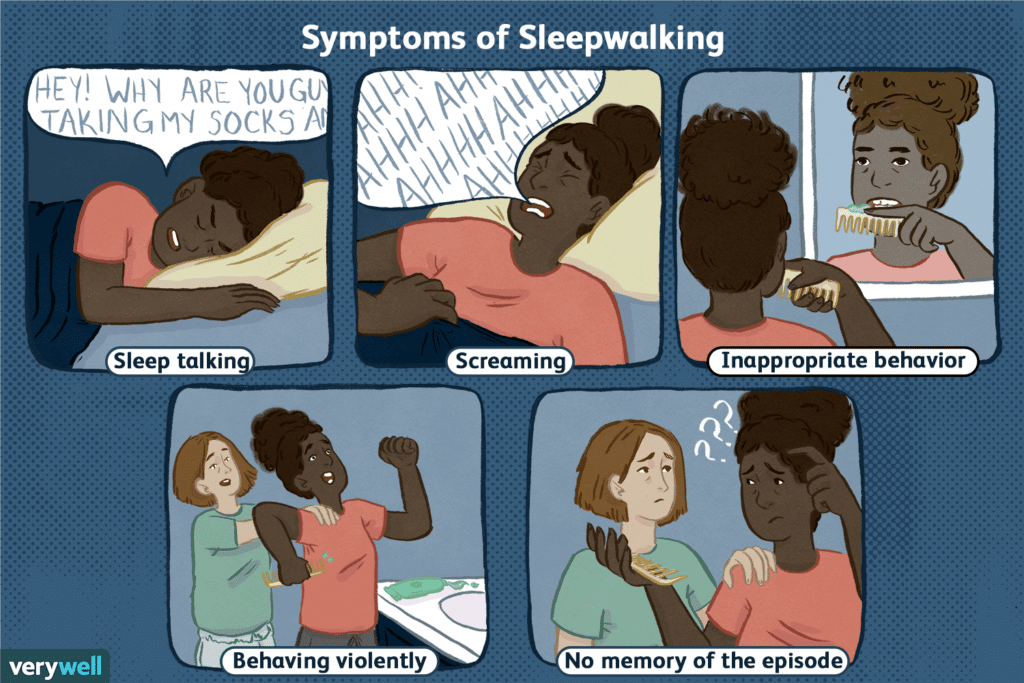
Sleepwalking is a type of parasomnia a sleep disorder that involves unusual behaviors during the sleep cycle. It typically occurs during the deepest stage of non-REM (NREM) sleep, usually in the first two to three hours after falling asleep. While it’s more common in children and often goes away with age, some adults experience sleepwalking due to various triggers or underlying conditions.
Should You Be Worried About Sleepwalking?
Sleepwalking isn’t usually dangerous by itself, but it can lead to risky situations. Imagine unknowingly walking down stairs, leaving the house, or even driving. It’s also worth noting that while many sleepwalkers are perfectly healthy, sleepwalking can sometimes be linked to other conditions.
Here’s a quick breakdown of potential causes and associations:
- Stress and Anxiety: High stress levels can trigger episodes.
- Genetics: Sleepwalking often runs in families.
- Sleep Disorders: Conditions like sleep apnea or restless leg syndrome can lead to disrupted sleep patterns, increasing the risk of sleepwalking.
- Mental Health Conditions: Disorders like depression, PTSD, and OCD can be linked to sleepwalking.
- Neurological Conditions: Alzheimer’s or Parkinson’s disease may contribute to sleepwalking in older adults.
- Medications or Substances: Certain drugs, alcohol, or even sleep deprivation can play a role.
How Does Mental Health Affect Sleepwalking?
Some mental health conditions can make you more prone to sleepwalking. For instance:
- Anxiety and Stress: Heightened emotional states can disrupt sleep and lead to episodes.
- Major Depressive Disorder (MDD): Changes in brain chemistry may contribute.
- PTSD: Trauma-related stress can manifest during sleep, including through sleepwalking.
- Schizophrenia: Though rare, some individuals may experience parasomnias like sleepwalking.
Conversely, sleepwalking can negatively impact mental health
- It can lead to poor sleep quality, causing daytime fatigue.
- Embarrassment or shame over sleepwalking behaviors can trigger social anxiety.
- Repeated episodes may disrupt relationships or daily routines, leading to depression.
Could Sleepwalking Be a Sign of Dementia?
In older adults, frequent sleepwalking might indicate underlying neurodegenerative changes, potentially linked to conditions like Lewy body dementia or Alzheimer’s disease. However, not everyone who sleepwalks will develop dementia.
Common Triggers and Risk Factors
| Trigger/Risk Factor | Description |
|---|---|
| Genetics | Family history increases likelihood of sleepwalking. |
| Stress and Anxiety | Emotional turmoil can disrupt sleep cycles. |
| Medications/Substances | Sedatives, antidepressants, and alcohol are common culprits. |
| Sleep Disorders | Conditions like sleep apnea often coexist with sleepwalking. |
| Neurological or Mental Conditions | Disorders like Alzheimer’s, PTSD, and depression may contribute. |
How to Manage and Prevent Sleepwalking
While sleepwalking isn’t always avoidable, you can take steps to reduce its frequency and ensure safety:
At Home
- Lock doors and windows: Prevent the sleepwalker from leaving the house.
- Clear hazards: Remove sharp objects, tripping risks, or breakables.
- Install alarms: Motion-sensitive alarms can alert you to movement.
Lifestyle Changes
- Stick to a regular sleep schedule.
- Reduce stress with relaxation techniques like meditation or yoga.
- Avoid alcohol and caffeine close to bedtime.
- Treat any underlying sleep disorders, such as obstructive sleep apnea.
When to See a Doctor
Consult a healthcare professional if:
- Sleepwalking occurs more than 1–2 times a week.
- There are signs of injury or dangerous behaviors during episodes.
- The sleepwalking begins suddenly in adulthood.
What to Expect from Diagnosis and Treatment
Your doctor may recommend:
- Polysomnography (Sleep Study): To track brain waves and identify other sleep disorders.
- Therapy: Cognitive-behavioral therapy (CBT) can help manage stress or mental health triggers.
- Medications: Sedatives or antidepressants might be prescribed in severe cases.
Conclusion
Sleepwalking might feel like a mysterious phenomenon, but it’s usually manageable with the right steps. By addressing triggers, improving sleep hygiene, and consulting a doctor when necessary, you can help reduce episodes and sleep more peacefully. If you or a loved one struggles with sleepwalking, don’t hesitate to seek support, it’s the first step toward a safer, more restful night.
FAQs
General Questions
Q: Is sleepwalking dangerous?
A: While not inherently dangerous, sleepwalking can lead to injuries, such as falls or accidents, especially if the sleepwalker encounters hazards.
Q: Can sleepwalking be cured?
A: Sleepwalking often resolves on its own in children. In adults, managing triggers like stress, sleep deprivation, or underlying health conditions can reduce episodes.
Q: Should I wake a sleepwalker?
A: It’s not harmful to wake a sleepwalker, but it may cause confusion. The safest approach is to gently guide them back to bed.
References
- Cleveland Clinic: Sleepwalking Causes and Treatment
- Mayo Clinic: Overview of Sleepwalking
- Healthline: Mental Health and Sleepwalking
- Sleep Foundation: Causes of Sleepwalking


